This is part of the Med in Small Doses series, which aims to give you a snapshot of a disease or disorder. For information about the series, or common abbreviations click here. Run through how to perform a neurological exam to refresh your memory, and link in clinical features.
F>M. Prev. 1/1000. Onset: 20-40yo. White matter lesions.
PATHO: Genetic & environmental factors. 15x risk in 1° relatives, 150x risk in MZTs. DH2 haplotype of MHC & other genes involved. Immune response against components of myelin sheath. Lesions separated in space and time. Initiated by CD4+ Cells. TH17 Cells → demyelination.
CFs: Unilateral optic neuritis. Cranial nerve signs. Motor and/or sensory impairment, fatigue, bladder & bowel symptoms. Need at least 2 neurological events separated in time &place.
DEMYELINATION
D iplopia / Dysmetria / Dysdiadochokinesis / Depression
E ye movement painful (Optic neuritis)
M otor: Weakness; spasticity
nYstagmus
E levation in temperature (Uhthoff's phenomenon)
L hermitte's sign
I ntention tremor
N europathic pain
A taxia
T alking is slurred; dysarthria
I mpotence
O veractive bladder (urinary urgency)
N umbness (sensory defect)
DEMYELINATION
D iplopia / Dysmetria / Dysdiadochokinesis / Depression
E ye movement painful (Optic neuritis)
M otor: Weakness; spasticity
nYstagmus
E levation in temperature (Uhthoff's phenomenon)
L hermitte's sign
I ntention tremor
N europathic pain
A taxia
T alking is slurred; dysarthria
I mpotence
O veractive bladder (urinary urgency)
N umbness (sensory defect)
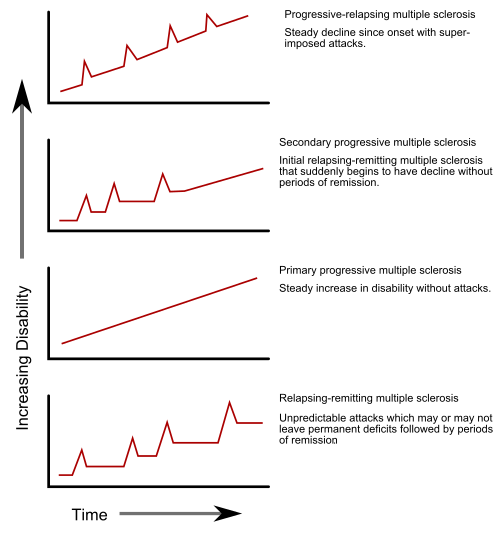
Types:
- Relapsing remitting (85%);
- Primary progressive (15%);
- Secondary progressive (progression from RR);
- Progressive relapsing.
MS Progression Types via Wikipedia
Ix: Plaques on MRI. CSF ↑ protein, pleocytosis, IgG, oligoclonal bands on electrophoresis.
Tx: No cure, aim to treat symptoms. Education, Physio, OT.
Acute: Methylprednisolone (high dose IV - 500mg, 5 days) or Prednisone (pts who Ø IV).
Plasma exchange.
Plasma exchange.
Relapsing: Interferon β, Galtiramir, Natalizumab.
Muscle spasticity: Baclofen, Botox, Diazepam







No comments:
Post a Comment